Features
Parents will worry, that is what parents do. But, according to Oxford Internet Institute researcher, Dr Matti Vuorre, the evidence base suggesting a negative impact of the use of technology on teenagers’ mental health is thin - at best.
Dr Vuorre and colleagues Dr Amy Orben and Professor Andy Przybylski have been studying the associations between technology use and adolescent mental health – and, according to new research, it is not all bad news, not at all.
It is popularly believed that new technology, particularly social media, is responsible for declining mental health among young people and a range of other social ills. But, says Dr Vuorre, concerns of this type are not new, nor are they well justified by current data.
Parents used to warn children that their eyes would turn square, if they watched too much television, and earlier generations were convinced listening to radio crime dramas...would inspire lives of crime
Parents used to warn children that their eyes would turn square, if they watched too much television, and earlier generations were convinced that listening to radio crime dramas, such as Dick Tracy (special agent) would inspire young people to turn to lives of crime.
Then, as now, says Dr Vuorre, the popular idea does not appear to be supported by hard evidence. The research, published last night, used data from three large surveys to look into the lives of more than 400,000 young people in the UK and US.
In these surveys, young people report on their personal use of technology and various mental health-related issues. Using this large data set, the team of researchers set about investigating the associations between adolescents’ technology use and mental health problems, and whether they have increased over time.
According to Dr Vuorre, these survey responses do not establish a smoking gun link between the use of technology and mental health issues, nor do they show that technologies have become more harmful over time.
‘We did find some limited associations between social media use and emotional problems, for instance,’ he says. ‘But it is hard to know why they are associated. It could be a number of factors [perhaps people with problems spend more time on social media seeking peer support?]. Furthermore, there was very little evidence to suggest those associations have increased over time.’
In fact, according to the new research, ‘Technology engagement had become less strongly associated with depression in the past decade, but social-media use had become more strongly associated with emotional problems.’
The study concludes, ‘The argument that fast-paced changes to social media platforms and devices have made them more harmful for adolescent mental health in the past decade is, therefore, not strongly supported by current data either.’
These results don’t mean that technology is all good for teens, or all bad, or getting worse for teenagers or not...it is difficult conclusively to determine the roles of technologies in young people’s lives
‘These results don’t mean that technology is all good for teens, or all bad, or getting worse for teenagers or not. Even with some of the larger data sets available to scientists, it is difficult conclusively to determine the roles of technologies in young people’s lives, and how their impacts might change over time.’
Dr Vuorre says. ‘Scientists are working hard on these questions, but their work is made more difficult by the fact that most of the data collected on online behaviours remains hidden in technology companies’ data warehouses.’
He adds, ‘We need more transparent research collaborations between independent researchers and technology companies. Before we do, we are generally in the dark.’
By Yu Shu
With the increasing demand for high-tech devices such as smart phones, wearable watches and portable health monitoring devices, the semiconductor manufacturing industry faces a big challenge of fabricating these devices in a sustainable and cost-effective way.
The current semiconductor manufacturing process releases a large amount of hazardous chemical waste in the fabrication process, which poses a great threat to human beings
The current semiconductor manufacturing process releases a large amount of hazardous chemical waste in the fabrication process, which poses a great threat to human beings (e.g., toxic chemicals may contain carcinogens) and the environment (e.g., resulting in water, oil and air pollution).
Compared to chemical waste management after the production, minimisation of the use of hazardous chemicals at the source is a more effective and sustainable approach to reduce the negative impact on the environment in long term. Thus the development of a water-based manufacturing technology becomes essential to the semiconductor industry.
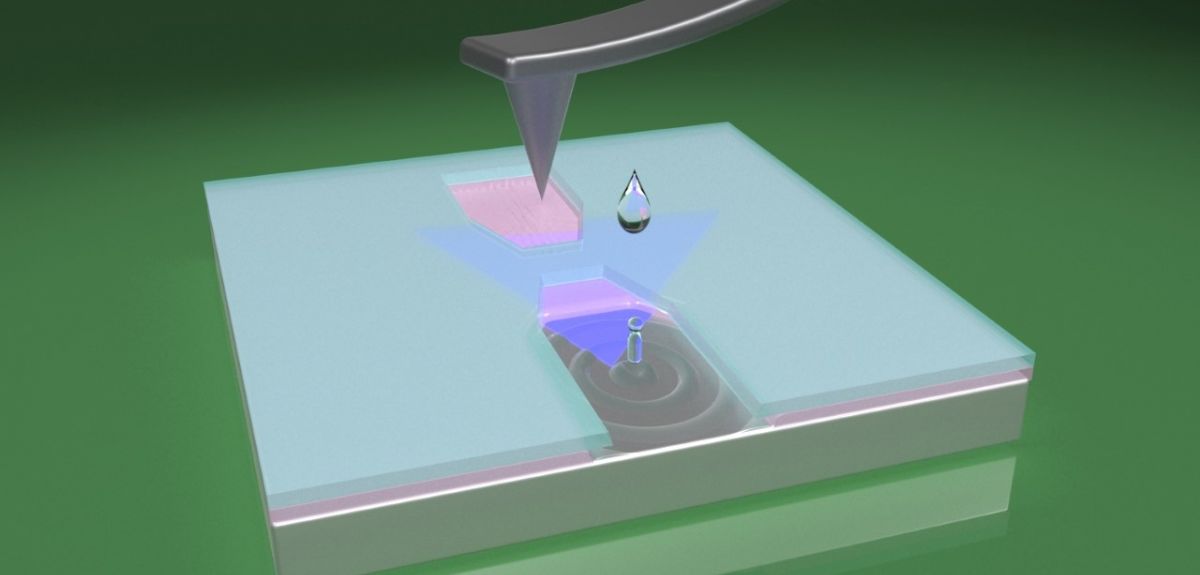
Recently we have proposed an environmentally friendly mechanical bilayer lithography approach that just uses water in the fabrication process. A nanoscale tip is employed to write patterns on the bilayer resist coated on the substrate of which one layer of resist is water soluble. This enables the water to act as the resist developer and remover and greatly reduces the use of chemicals at the source.
Recently we have proposed an environmentally friendly mechanical bilayer lithography approach that just uses water in the fabrication process
Compared to conventional photolithography techniques that use a lot of organic solvents in the fabrication process, the water-based process shows great sustainability with reduced influence of chemical wastes on the environment. Based on the fact that the key parts of smart devices are complex integrated circuits, this approach has the substantial potential to be utilised in semiconductor manufacturing as it is capable of writing various patterns in both nanoscale and microscale. The highest achievable resolution is 310 nm, with the scope of further improvement.
The water-based approach is applicable to a wide range of materials especially sensitive materials such as polymers and two-dimensional materials. This also brings a lot of opportunities in flexible and wearable technologies. Polymers with low cost, light weight and flexibility are promising flexible substrates, while two-dimensional materials that have atomic thickness and great electronic and photonic properties can be seamlessly integrated with flexible substrates.
The water-based approach is applicable to a wide range of materials especially sensitive materials such as polymers and two-dimensional materials
However, they both have the disadvantage of low resistance to chemical and radiation damage. This research gives a demonstrator of a flexible MoS2 photodetector fabricated by the water-based mechanical bilayer lithography technique. Due to the protection from chemical and radiation damage, the flexible photodetector shows a rather rapid photoresponse of 42 ms to the red laser diode with the wavelength of 633 nm, validating the superior functional applicability of the water-based process.
This research work is led by Professor Harish Bhaskaran in Department of Materials at Oxford University and is funded by EPSRC Wearable and Flexible Technologies programme. More information about the work can be found in the full paper published in Nano Letters - 'Nanoscale Bilayer Mechanical Lithography Using Water as Developer'.
Yu Shu is a DPhil student at the Department of Materials and co-authored the above paper.
Every year, thousands of babies around the world are born with rare genetic diseases leading to death or lifelong disability. With technological advancements in the fields of genetics and medicine, the rate of introduction of treatments for these rare conditions has grown remarkably.
Interestingly, new treatment costs can range from very little to several million pounds. A recently approved Spinal Muscular Atrophy gene therapy has been priced in the UK at ~£1,8m. Several devastating diseases affecting children can be treated with very cheap drugs and even vitamins. For example, Congenital Myasthenia may cause deep hypotonia (decreased muscle tone) and respiratory insufficiency, where the body is not provided with enough oxygen. It is a rare disease, and the patient’s journey to diagnosis can be extremely long. Nevertheless, Congenital Myasthenia can be dramatically improved with salbutamol or pyridostigmine, two very cheap drugs.
All of this could have been avoided with an early diagnosis and a simple drug costing about £7 a month.
Before moving to the UK, I diagnosed three patients with DOK7, causing muscle weakness, in my hometown of Liège, Belgium. The three patients spent 60 years collectively in a wheelchair, had six muscle biopsies that were not helpful, and spent 45 years with invasive ventilation. All of this could have been avoided with an early diagnosis and a simple drug costing about £7 a month.
Last week I diagnosed a child with a neurotransmitter disease. This baby boy, now 18 months old, is in a severe condition that would have responded quickly to L-dopa, folic acid and serotonin, all cheap medications. Today, after several long and severe epileptic seizures, it is likely too late. A variety of severe epileptic disorders of newborns, leading to irreversible damage to the brain, are readily treatable with pyridoxine, or pyridoxal phosphate, two cheap vitamins.
There are many more examples like these. Many more stories of lifetimes spent in a wheelchair, many more stories of patients connected to a respirator long term, families exhausted by diseases that we could have diagnosed and treated much earlier.
Timing is of great importance
Early diagnosis is of primary importance both to obtain the best effect of innovative medications and to accelerate their development.
In nearly all of these rare diseases, timing is of great importance for medication administration. The benefit for a patient who has already suffered from a long, irreversible disorder is small and, sometimes, hardly justifies the cost and the burden of the treatment. Early diagnosis is of primary importance both to obtain the best effect of innovative medications and to accelerate their development. Early diagnosis is easily achievable by universal newborn screening (NBS).
NBS has existed for more than 40 years, but has focused on metabolic diseases like phenylketonuria. All the diseases mentioned here are probably even better candidates for newborn screening than phenylketonuria, which is the “archetype” of diseases that warrant newborn screening. The only difference is the methods that are now used.
In 2018, we pioneered an innovative genetic NBS programme in Southern Belgium for Spinal Muscular Atrophy (SMA) that has, so far, allowed nine children to be diagnosed and treated early and avoid the terrible fate of the disease. The programme was rolled out in 16 countries, including public dissemination and health-economic analysis from the beginning. Very recently, SMA officially entered the NBS programme in Belgium.
Being much more efficient in the diagnosis of treatable conditions and in the treatment of these diseases is feasible. It needs funding and open minds.
In the UK, we have designed and funded a pilot study that aims to screen 24,000 newborns/year and for which we are currently seeking approval. When you know that every five days a child is born in the UK with this disease and will at best spend their life in a wheelchair, rather than being able to walk if diagnosed at birth, the waiting is difficult.
Being much more efficient in the diagnosis of treatable conditions and in the treatment of these diseases is feasible. It needs funding and open minds. We need to ask ourselves the basic question, “Why not?”. We must place ourselves in the shoes of parents and ask ourselves: if there is a test to find if my child has a treatable disorder and to fix it immediately, rather than taking the risk of waiting for the disease and irreversible damage, why would I not take it?
Further information can be found at:
NHS information of newborn screening
Professor Laurent Servais is Professor of Paediatric Neuromuscular Diseases at the MDUK Oxford Neuromuscular Centre and Invited Professor of Child Neurology at Liège University. He leads numerous clinical trials in neuromuscular diseases and has a special interest in newborn screening programmes.
By Dr Samantha Vanderslott, Oxford Martin School and Dr Seilesh Kadambari, Department of Paediatrics
Why is this important to us?
We have been struck by how COVID-19 has affected the health and wellbeing of ethnic minority groups disproportionately. Individuals from these communities are more likely to have severe disease requiring intensive care admission and sadly succumb to infection than those from a white ethnic background. This is independent of age, gender or socioeconomic factors. However, vaccine uptake has been low in certain communities and for lots of different reasons. These include specific concerns about vaccine safety, increased exposure to misinformation, reduced access to vaccines and historical distrust with institutions. Asylum seekers have cited negative experiences with authorities, and some don’t trust public health messaging related to vaccines. Central government often use one-way messaging, which will sometimes miss these groups. Promoting vaccination through celebrity adverts, videos via social media and community champions may also not reach disaffected communities who feel marginalised during the pandemic. We encourage a two-way dialogue in the hope that these groups can trust us with providing evidence-based answers to queries and enable informed decision making before getting a vaccine.
What are we doing?
We found approximately 200 community organisations online that provide community, religious or social support to individuals and groups across the UK. We approached these organisations to invite us to any online meetings being held during the lockdown in order to provide information about the vaccine, answer questions and encourage dialogue. Our intention has been not to overwhelm individuals with information and so we do not use slides or overly scientific language. The majority of our meetings are therefore spent listening to concerns or questions, addressing these directly and encouraging two-way conversation.
We have spoken to organisations that support asylum seekers, refugees, interfaith groups and elderly ethnic minority citizens. Concerns have ranged from the risk of deportation by registering for a vaccine, addressing misinformation that has circulated in specific communities and discussing a range of vaccine safety concerns.
Who is involved?
This initiative is conducted by Dr Seilesh Kadambari and Dr Samantha Vanderslott. We are based at Oxford Vaccine Group and use information and materials from the Vaccine Knowledge Project.
The Vaccine Knowledge Project has also worked with the British Islamic Medical Association to develop FAQs about vaccines and vaccine ingredients translated into over 100 different languages and available on the website. This resource has been shared through these online conversations and their communities. The calls are facilitated by the organisations that we have reached out to. We have benefited from having a medic able to address safety issues and health conditions and a researcher able to address vaccine policies and misinformation.
What works for us?
Most importantly, this work has highlighted the importance of connecting with individuals and groups directly. We ensure that every opportunity is taken to answer questions and that individuals can make an evidence-based decision on whether to receive a vaccine. The meetings, facilitated by community leaders, are held at convenient times for different organisations. For example, in the afternoon for an organisation supporting elderly women of South Asian background, in the evening after work for a group supporting asylum seekers and on a weekend before Ramadan for Muslim organisations. It has been deeply humbling and thoroughly enjoyable work. Our aim has been to provide individuals with sufficient confidence to receive a vaccine and therefore ensure protection against a pandemic that has exacerbated disparities in these vulnerable groups.
More information
For information and materials on vaccination, check out the Vaccine Knowledge Project.
There are also plenty of other examples of good practice.
When will this all be over? As the number of COVID-related infections, hospitalisations and deaths reported in the UK continues to fall, the chorus grows ever louder for the abandonment of restrictions on everyday activity.
Summer holidays in Spain, crowded sporting arenas and nightclubbing, are held out as examples of normal life to which we can look forward. But, for many, it is the more mundane life they miss: meeting friends and relations indoors, having a coffee in a coffee shop, going to the library or cinema.
But the question of when the pandemic (or epidemic) is over is not as simple as it might appear. It is a medical question, but determining what is an epidemic and when it has ended is also a political and social question.
In the past, epidemics have ended in a variety of ways...sometimes the illness has gone but sometimes people have learned to live with it
In the past, epidemics have ended in a variety of ways – some in which the illness has gone and others in which it has not, but people have learned to live with it.
Oxford Historian Dr Erica Charters is leading a project looking at these complex questions. Some 40 researchers, from more than a dozen universities across the academic spectrum, have come together to study - ‘How Epidemics End’.
The team includes experts in a variety of past events which have wreaked havoc around the world – from the plague to TB to HIV/AIDs to cholera.. And this week the team is releasing a series of videos discussing what has happened in past epidemics. The first three videos compare how different researchers study cholera and its ending, explaining the cholera epidemics which devastated countries including England in the 19th century, but more recently, Yemen.
‘We have asked the question: how did epidemics end?’ says Dr Charters. ‘We have brought together longer term reflections on this and looked at the different ways of distinguishing the end – looking at epidemiological and mathematical models alongside political and social questions.
’But there is no one answer. Everyone wants certainty and answers but it is not just a decision about a disease but a political decision: what will people live with?’
Everyone wants certainty and answers but it is not just a decision about a disease but a political decision: what will people live with?
Dr Erica Charters
In January, Dr Charters and Dr Kristin Heitman wrote, ‘Detailed research on past epidemics has demonstrated that they do not end suddenly; indeed, only rarely do the diseases in question actually end.’
Dr Charters points out, ‘In the past, epidemics have ended in one of three ways.
‘People begin to live with it [influenza]. It moves to another part of the world [the plague] or it is managed through medical treatment and no longer seen as an epidemic in that part of the world [HIV/AIDs].’
As the numbers of infections continue to fall in the UK, although other countries are still experiencing severe illness, COVID appears to follow the pattern. But Dr Charters warns against ‘false endings’. And the historian, who specialises in the history of medicine, points out that some diseases may be considered an epidemic in some parts of the world but may be common elsewhere, ‘Malaria is endemic in large parts of Africa but if there were cases in England, it would cause alarm.’
People begin to live with it [influenza]. It moves to another part of the world [the plague] or it is managed through medical treatment and no longer seen as an epidemic in that part of the world [HIV/AIDs]
It is this sense of alarm which underpins the pandemic (which is an epidemic on a global scale). The January paper maintains, ‘Epidemics—like the recurring narratives they produce—throw a society's confusion, fears, and anxieties into high relief.’
It continues, ‘When communities are thrown into panic and turmoil by the outbreak of a new disease, when medical committees are convened and central governments spring into action, epidemics are understood in clear biological terms.... But at the end stages of epidemics, the disease is regarded through the filter of political, social, and economic dislocation—dislocations that have deepened as the epidemic progressed—articulating the processes by which policy decisions are debated and implemented, and the accommodations between scientific models and human behaviour.’
The World Health Organisation categorises it as a public health emergency of international concern. But, from a global perspective, it means different things to different groups at different times – not just as the disease spreads around the world but because within the same country, different groups will experience a disease differently.
So the end will also be different for different peoples. Dr Charters says, ‘It is unlikely that there will be a single end date.’
There may be biological markers, suggesting a decline in infections or excess deaths. People tried to track these in 17th century England, when the number of plague deaths fell and the population returned to London – rather prematurely.
But, says Dr Charters, in general, the end of epidemics can be traced to ‘when people resume social practices’. She adds, ‘When the city gates opened and groups returned.’
In general, the end of epidemics can be traced to when people resume social practices. When the city gates opened and groups returned
And she notes, there is also a falling off of evidence – as people stop recording the impact of the disease and go back to their previous occupations.
According to the article ‘How epidemics end’, ‘Epidemics end once the diseases become accepted into people's daily lives and routines, becoming endemic—domesticated—and accepted. Endemic diseases typically lack an overarching narrative because they do not seem to require explanation. More often, they appear as integrated parts of the natural order of things.’
But, says Cr Charters, one of the research team points out that there have just as often been celebrations and thanksgiving to mark the end of epidemics - that they have not just fizzled out.
Endings were not always quiet,’ she says. ‘There have been celebrations and fireworks, thanksgiving...but most epidemics have ended when people just returned to their lives.'
See the videos here How epidemics end | How Epidemics End (ox.ac.uk)
- ‹ previous
- 26 of 252
- next ›




 What US intervention could mean for displaced Venezuelans
What US intervention could mean for displaced Venezuelans  10 years on: The Oxford learning centre making an impact
10 years on: The Oxford learning centre making an impact Oxford and The Brilliant Club: inspiring the next generation of scholars
Oxford and The Brilliant Club: inspiring the next generation of scholars New course launched for the next generation of creative translators
New course launched for the next generation of creative translators The art of translation – raising the profile of languages in schools
The art of translation – raising the profile of languages in schools  Tracking resistance: Mapping the spread of drug-resistant malaria
Tracking resistance: Mapping the spread of drug-resistant malaria