Improving survival rates of childhood blood cancer in Africa
Oxford researchers are working with colleagues in sub-Saharan Africa to change a 90% death rate, into a 90% cure rate.
According to the World Health Organisation, cancer is a leading cause of death for children and adolescents worldwide, with blood cancers such as leukaemia and lymphoma being the most common. In high-income countries more than 80% of children with cancer are cured, but in many low- or middle-income countries, only 20% are cured.
Childhood blood cancer kills thousands of children every year in sub-Saharan Africa. A subsection of blood cancers known as Epstein-Barr Virus-related lymphomas (or EBV lymphomas) are particularly deadly, and have become the focus of a new international global health collaboration which hopes to improve EBV lymphoma treatment and diagnosis, AI-REAL (Aggressive Infection-Related East Africa Lymphoma).
Traditional but painful and expensive diagnostic procedures, such as invasive needle biopsies, are currently more commonly used in sub-Saharan Africa due to a lack of advanced equipment. Only 29% of hospitals in Tanzania and Uganda have the required surgeons to perform these procedures.
As a result, many children are going undiagnosed and untreated leading to an astonishing 90% death rate from EBV driven lymphomas. But through improved equipment, training and access to advanced diagnostic technologies, AI-REAL aims to turn this 90% death rate into a 90% cure rate.
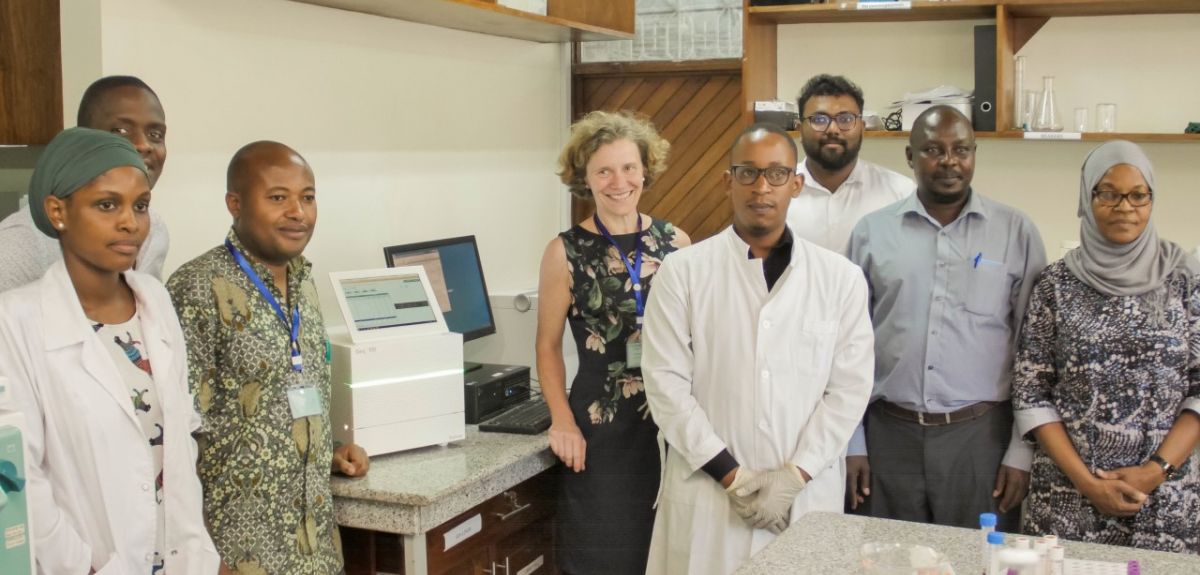
Professor Anna Schuh, Professor of Haematology at the University of Oxford leads this new UK-Africa project, which aims to bring the next generation of diagnosis technology to Tanzania and Uganda. Prof. Schuh hopes the in-country testing process for EBV lymphomas can be further developed, in order to improve early diagnosis and chances of survival.
Schuh says, ‘There are currently 43 pathologists in Tanzania for 56 million people alone, so there is a big need to improve the capacity for early diagnosis through access to diagnostic software and training. By bringing in these new technologies we hope to train the future generation of clinicians and scientists to speed up diagnosis and improve the lives of millions of children in sub-Saharan Africa.’
Professor Schuh and her team will be visiting Africa during the duration of the project to provide training in various techniques and equipment, such as next generation genetic sequencing technology and artificial intelligence tools, with the hope of minimising patient pain and delivering faster diagnoses.
By sharing these best practices and bringing the latest technological advances in genetic testing in country, it is possible to set up effective and affordable cancer diagnostics through the use of simple blood tests to screen for cancer.
This project was launched in February 2020, and is a partnership between the University of Oxford and medical teams in the Muhimbili National Hospital, Kilimanjaro Christian Medical Centre, St Mary’s Hospital (Lacor) and Muhimbili University of Health and Allied Sciences, with funding from the NIHR RIGHT Programme. September is Blood Cancer Awareness month. To find out more about blood cancers, visit the Blood Cancer UK website.