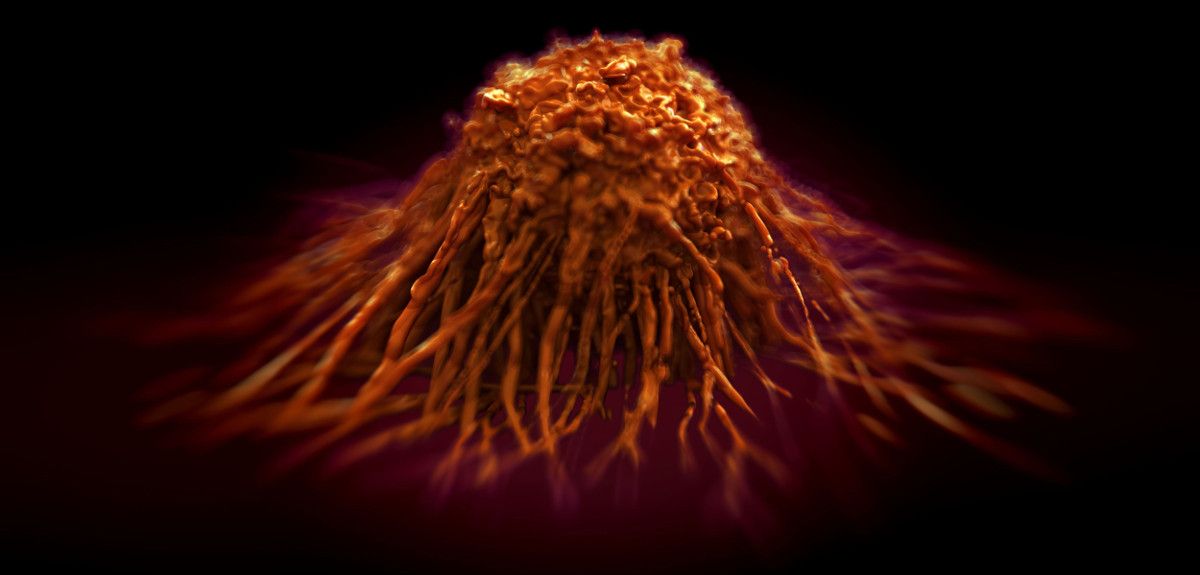
Image credit: royaltystockphoto.com/ Shutterstock
The future of cancer treatment
1 in 3 people born after 1960 in the UK will be diagnosed with some form of cancer in their lifetime, and each year, 4th February marks World Cancer Day, to raise awareness and encourage individuals and governments to fight the disease.
Oxford University has many research groups working at the cutting edge of the fight against cancer, and I spoke to one such researcher, Professor Colin Goding from the Ludwig Institute at the Nuffield Department of Medicine, about what cancer treatments might look like in the future.
We have something like 14 million million cells in our body, but only one in three of us, and over many years, gets cancer.
Professor Colin Goding
Oxford Science Blog: Why is cancer of interest to scientists?
Colin Goding: We have something like 14 million million cells in our body, but only one in three of us, and over many years, gets cancer (defined by the uncontrolled division of cells which grow to form tumour). At the cellular level, cancer is extremely rare, and this is because we have mechanisms that block mutated cells progressing towards disease.
We study these mechanisms in melanomas, which are cancers that begin in melanocytes – the cells the produce the pigment melanin, which colours skin, hair and eyes. So melanomas are usually (but not always) skin cancers.
Melanoma are a good ‘model’ for cancer because we can see all stages of the disease: completely normal pigment cells, but also moles that have an activated cancer-causing gene that puts its foot on the ‘accelerator’ pushing cells to divide, counterbalanced by a very strong anti-cancer mechanism (present in all cells) that cuts the fuel to the engine so cells stop dividing.
We can also see melanomas that progress to spread across the surface of the skin, or those that start to invade and spread to other parts of the body. We’re particularly interested in how these state changes happen.
OSB: Given the rarity of the cellular events that lead to cancer, how does it ever take hold?
For 50 years, there was very little progress in treatments for melanoma.
Professor Colin Goding
CG: It is a complicated process, but to get a cancer, you need to inactivate the ‘brake’ that stops uncontrolled cell division, and there is more than one cellular braking system. On top of this, the genes encoding the ‘accelerator’ for cell division have to be turned on.
If these mutations occur in the wrong order, the engine stalls: there is no cancer. To get cancer, the mutations need to happen in the correct order: you lose the ‘brakes’, the cell machinery gets put in gear, and then the ‘accelerator’ mutations happen. Only then will the cancer progress.
OSB: Why are you particularly interested in melanomas?
CG: The advantage of studying melanomas is that, as a skin cancer, we can see all of these disease stages – in lung cancer, for example, by the time a patient comes in with symptoms, the cancer has usually already moved to quite a late stage.
There are now new drugs in the clinic that will help reactivate the immune system, enabling it to attack the cancer.
Professor Colin Goding
Another advantage of studying melanomas is that we understand a lot about the genetics of pigment cells, and many of the genes that have gone wrong in melanoma are the ones involved in the normal development of pigment cells. So we have a pretty good understanding of the genetic basis of this form of cancer: we know that the ‘accelerator’ genes are, for example, and we understand the braking mechanisms too.
Melanoma is also a form of cancer that affects many people: there are over 13,000 new cases of melanoma every year. The measure that correlates best with disease rates is childhood sunburn and cases of melanoma have been doubling every 10 years for the last 40 years. This is partially because there is about a 30 year lag between people becoming aware of the dangers of UV exposure from the sun and a change in disease rates.
And it is still the case that if you go to a park on a hot sunny day, or the beach, there are still people who are getting burnt. So there is still work to do in educating the public about the dangers of excessive sun exposure.
OSB: How has the treatment for melanoma changed over these decades?
CG: For 50 years, there was very little progress in treatments for melanoma: surgery to cut out early lesions before they started to spread is still a very effective therapy, but that was pretty much it.
But the realization that certain genes act as the accelerator pedal to push melanoma formation has led to drugs that target this mechanism. We now know which cancer gene responds to which particular drug. The response in patients whose cancer stems from these sorts of mutations is very good, but if the patient does not have the specific gene targeted by that drug, treatment with that drug might actually make things worse. So patients are now increasingly being tested for particular mutations before being treated with specific drugs.
The real problem, however, is that even if a drug works, for most patients, it is almost inevitable that resistance to that drug also appears some months later: the drug stops working, and the cancer carries on growing and spreading, eventually killing the patient.
A huge amount of work over the last 50 years or so has also gone into understanding the mechanisms cells use to block immune cells from infiltrating and attacking a developing tumour. Many of these mechanisms have now been identified, and the consequence is that there are now new drugs in the clinic that will help reactivate the immune system, enabling it to attack the cancer.
These drugs have also been very effective in many patients, but again, not all patients respond, there are many side-effects, and in some cases, resistance sets in after a while.
Essentially, resistance seems almost unavoidable for any one single kind of drug.
OSB: What can be done to combat this resistance?
CG: The first mechanism for cancer drug resistance is genetic: unless the disease is at a very early stage, within all the cancer cells in a patient’s body there is likely to be at least one that has another mutation that confers resistance to a particular drug or therapy. So when that drug is used, all of the other cells die, but the one with the mutation survives – and it then repopulates the tumour. This turns out to be quite a common mechanism for resistance to so-called targeted therapies that hit a key molecule.
The only way to really deal with this mechanism of resistance is to treat the patient early, and when the treatment is successful, to monitor the patient very carefully, with tools that are more sensitive that those we currently have, to track the cancer coming back.
This is because it’s a numbers game for genetic resistance - the chances of resistance developing are proportional to the number of cancer cells in the body. The greater the number of these cells, the greater the likelihood that some cells will be resistant to the drug being used. So even if you have a second drug that can kill cancer cells that survive the first drug, giving the second drug at a later stage, when there are many more cancer cells, means that it is again almost inevitable that a few cells will be resistant to the second drug too.
So treating as early as possible, when there are as few cancer cells in the body as possible, is the best way of overcoming genetic resistance.
OSB: How does your own work approach these treatment failures?
CG: We work on the second mechanism for cancer resistance, one based on the cancer cells in a tumour adopting different states.
We and others have found that in different circumstances, cancer cells can adopt different ‘personalities’ that can be more or less resistant to a particular treatment. The adoption of these different states is influenced by the microenvironment surrounding each cell, which includes factors like oxygen or nutrient levels, or signals from infiltrating immune cells.
All of these factors combine to induce the tumour cells to adopt different states. One of these states might be a drug-resistant state, another might be an invasive state, where cells start to move away from the primary tumour and spread throughout the body to form metastases.
For example, we now know, from the work that we’ve done on melanomas, that movement away from the primary tumour to seed these metastasis is primarily driven by the cancer cells’ microenvironment.
The interesting thing is that the cancer cell states are dynamic and reversible, and these micro-environmental influences can potentially be modulated by drugs. This isn’t quite the case for the genetic mutations, which are pretty much irreversible – you can target the altered protein made by the mutation, or you can try and kill the mutated cells when their numbers are low, but that’s the only way you can deal with the genetic issue in cancer.
But by understanding cancer cell states, we can perhaps turn a drug-resistant population of cells to a drug-sensitive one.
OSB: How could you bring about this change in state?
CG: We could do this by changing the micro-environment, or by finding drugs that drive cells to adopt a particular state. We’ve done this quite successfully for a drug called methotrexate – this was already in use for psoriasis and rheumatoid arthritis, but we found out a couple of years ago that this drug switches on one of the genes that stops melanoma cells spreading to other parts of the body. Working in collaboration with another group, we also found that methotrexate also sensitized cancer cells to another drug, and so we’re currently working on ways to drive cancer cells into states responsive to different drugs.
We think many drugs designed for other diseases and not currently used to treat cancer might turn out to be useful for targeting some of these mechanisms which can switch cancer cells from one state to another.
OSB: How do you think cancer therapies need to change in the future?
CG: Cancer therapies need two things: first, we need to identify relapse (the cancer coming back) way ahead of when we do now, so that drugs that can bypass resistance to the first therapy can be given before resistance to the second therapy arises. This is similar to what we already do for bacterial infections: we don’t use the same antibiotic again when a first dose leaves resistant bacteria, and we ideally give a second antibiotic before the infection becomes re-established.
The second approach needs us to really understand the mechanisms by which cancer cells adopt inter-convertible states with different drug sensitivities. Then, we can use drug combinations, so that drug A sensitizes a tumour to drug B. We need to be really clever about how to do this and get the timing right. This requires quite a lot of work to understand fully the processes involved, but we’re getting there!