Features
Researchers from the University of Oxford have been sharing their work with the public at the Royal Society Summer Science Exhibition (1-7 July 2019).
Breathe Oxford is a diverse group of neuroscientists, psychologists and clinicians studying the neuroscience of breathlessness. Their work shows that breathing is about more than just the lungs. In fact, the brain has a powerful influence on our experiences. This explains why some people still feel out of breath, even when they have been provided with medical care.
They explore how the brain controls our feelings of being out of breath using cutting-edge brain imaging technology. Understanding this control system could lead to revolutionary, personalised treatments for breathlessness.
Their exhibit at the Royal Society Summer Science Exhibition will bring the topic of ‘Breathing with your Brain’ to life, helping visitors to understand the how the brain controls our feelings of being out of breath.
Researcher and lead organiser Dr Sarah Finnegan said: 'Our research has shown the power of the brain-body interaction in influencing how we perceive our breathing.
'This is a relationship that we are only now just beginning to understand, and we hope eventually to develop target treatments for individuals, helping millions of people who are limited by their breathlessness.
'We are thrilled to be able to share some of the cutting-edge neuroscience that takes place at Oxford with visitors to the Royal Society, and hopefully we can inspire some future scientists!'
It is estimated that one in nine people experience some form of breathlessness, which is most common in conditions such as heart failure, lung disease, panic disorder and Parkinson’s. But there are also significant numbers of people who have unexplained breathlessness, which Breathe Oxford hypothesise might be driven by the networks in the brain.
Breathe Oxford has examined breathlessness in athletes, healthy individuals and people with chronic lung disease, seeking clues as to why some individuals become disabled by their breathlessness, while others, with the same lung function, live normal lives.
Visitors to the exhibit will be able to simulate living with chronic breathlessness by exercising on the ‘Steppatron’ with a straw in their mouth and a clip on their nose. They will also be able to witness the brain’s relationship with breathing on a 3D-printed scale model of a human torso with breathing lungs and LED lights which will highlight the neural pathways between the brain and the lungs. A specially commissioned animation will also reveal more about the background to the science.
Other stalls at the Summer Exhibition this year that involve Oxford research are:
Robots in the Danger Zone - Dr Maurice Fallon and others from the Department of Engineering Science's Oxford Robotics Institute will be demonstrating their research into robotics for inspection of dirty, dull and dangerous places, specifically with walking robots, such as their quadruped ANYmal. The stand is being presented by the ORCA Robotics Hub. See a video of the group's work here.
Living on the Moon! - an interactive experience highlighting the progress of lunar science since the Apollo 11 Moon landings 50 years ago. The exhibit illustrates the journey from Moon landing, to Lunar sample science, to the current generation of Moon rovers looking for water on the Moon, and provides a look forward to the next 50 years and a vision of a permanent human presence on the Moon. (Researcher: Dr Neil Bowles from the Department of Physics.)
In Your Element - 150 years of the periodic table: Investigating the elements that are essential to life. Biogeochemists from the Department of Earth Sciences' OceanBug team are presenting the journey of elements from the earth’s crust through the ocean and ultimately to feed life throughout Earth’s history. The exhibit is led by the University of Warwick.
Professor Kyle Pattinson from the Nuffield Department of Clinical Neurosciences explains how brain scanning could help doctors to personalise treatment for people with chronic breathing disorders.
Ever realised you’ve forgotten your inhaler and immediately felt your breathing become more difficult? Ever wanted to walk upstairs to get something, but the thought of becoming breathless has stopped you? You’re not alone! Our brains store a phenomenal amount of information about the world, based on our past experiences. This helps us to assess situations quickly and anticipate how our bodies will respond, such as when we will become breathless. These ideas are learned and updated constantly throughout our life, and quickly adapt if we develop something like a chronic breathing disorder.
These learned ideas, or ‘priors’, are thought to not only influence our actions (such as avoiding the stairs), but can materially alter the way we perceive a symptom like breathlessness. This theory is termed the ‘Bayesian brain hypothesis’, and it explains how our priors are compared to incoming sensory information in the brain, and both pieces of information are used to create our conscious perception.
Breathlessness can be experienced by people with a wide range of conditions: those with respiratory, cardiovascular or neuromuscular diseases, as well as some people with cancer or conditions such as panic disorder. Symptoms vary, but can include hunger for air, increased breathing effort, rapid breathing and chest tightness. These breathing symptoms have been known for a long time to be influenced by psychological states such as anxiety, but also by low mood, hormone status, gender, obesity and level of fitness. However, the influence of our previous experiences and learned associations has only more recently entered into the equation.
When we have repeated or frightening exposures to breathlessness, such as an asthma attack or severe breathlessness, our brain can quickly learn and update our priors. This system is designed to help us to avoid threats and keep us safe, but generating very strong expectations (priors) about breathlessness can then exacerbate our symptoms on future occasions. What’s more, certain personailty traits such as higher anxiety, or greater body awareness may also influence this system, making some people more susceptible to developing strong expectations about their breathlessness. Once these expectations are embedded, they can be difficult to ‘un-learn’ – the brain can easily catastrophise about the potential worst case scenario, such as having another asthma attack.
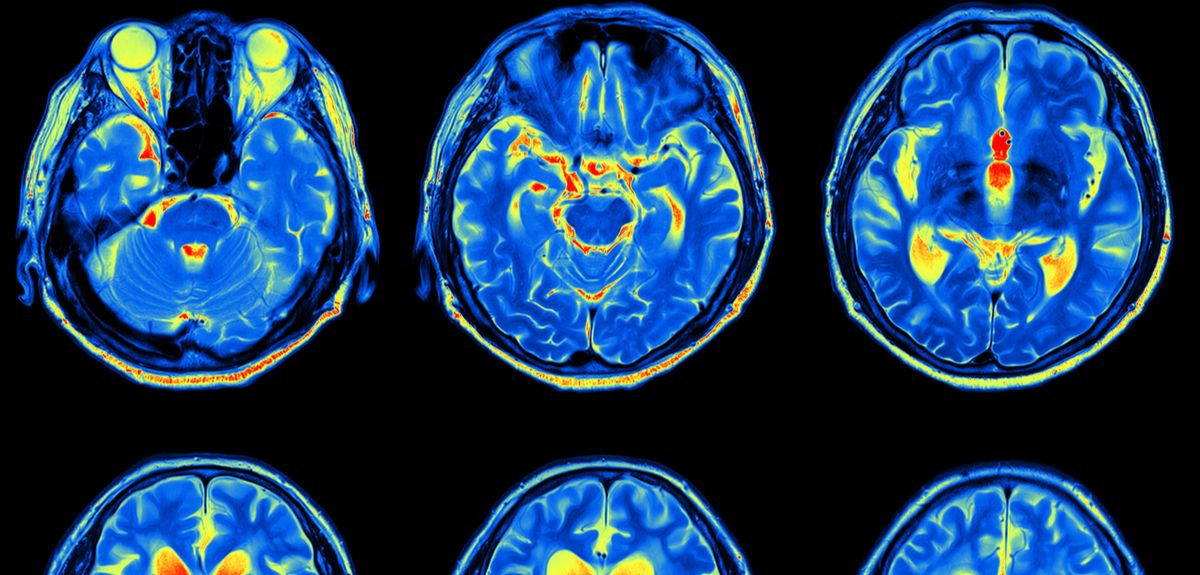
Scientists at the University of Oxford are at the cutting-edge of a continually improving brain imaging technology that is being used to shed some light on what exactly is happening when we anticipate and experience breathlessness (see some examples here and here). Over the last eight years our research team has been steadily chipping away at these brain mysteries, in the hope that their findings will lead to more carefully targeted and personalised treatments for people with chronic breathlessness.
In the Nuffield Department of Clinical Neurosciences, we are using high-field functional magnetic resonance imaging to look at the brain’s workings in incredible detail. This has enabled us to start uncovering the complex neural mechanisms involved in dealing with breathlessness.
The team have been exploring brain networks of breathlessness perception in people with chronic obstructive pulmonary disease (sometimes known as emphysema or bronchitis). The most successful currently available treatment for this condition is pulmonary rehabilitation: a programme of exercise, education, and support to help people with chronic breathing problems learn to breathe more easily again. This type of rehabilitation does not influence physical lung function. That means that it must instead work by helping people to change their learned priors, which make them overestimate the threat of breathlessness (we’re back to those stairs again).
Using functional magnetic resonance imaging, we have confirmed that the people who had benefitted from this rehabilitation programme had both higher initial brain activity and greater rehabilitation-induced changes in parts of the brain linked to body symptom evaluation and emotion – the insula and anterior cingulate cortex. They are now working towards studies that can help to increase these changes in breathlessness expectations, and to identify which people in particular are most amenable to the benefits of pulmonary rehabilitation. This was the focus of our recently published study, and will help to better understand how personalised therapy may be designed for each individual.
Treating the lungs AND the brain
Clearly there can’t be a ‘one size fits all’ approach to treating debilitating perceptions of breathlessness. Current attempts to treat the complexity of chronic breathing problems have been somewhat scattered, and we must now work towards understanding the individual ‘lived experience of breathlessness’ to lead us to more carefully nuanced interventions. The different factors at play in breathlessness all need to be targeted as part of a comprehensive treatment programme: What are the brain mechanisms at work in learned expectations? How do anxiety, stress and low mood impact on breathlessness? How closely are the observable physical symptoms actually linked to lung function? Imagine the discomfort that could be reduced and quality of life that could be improved, not to mention the money that could be saved (breathlessness due to COPD costs the NHS more than £4 billion per year), if breathlessness were approached in a more holistic way.
Pulmonary rehabilitation is just one in a raft of potential behavioural and drug therapies that could be used to ease the often crippling fear of breathlessness. Only 35% of people who are prescribed pulmonary rehabilitation actually take it up (for a variety of reasons, including not being able to get out to the venues where it is run); and only 60% of those who take it up actually benefit. Therefore, more research is needed to understand the specific mechanisms of breathlessness perception, and develop different treatments that would be suitable for different people. It is the details we are gleaning about the incredibly complex brain mechanisms of symptom perception that will equip us to design more successful treatment options for those whose symptoms do not match their lung function, to bring breathlessness back under control.
'It became very hard to breathe…but I just had to remember to keep calm and still.'
You might be thinking that this sounds like a hapless victim from one of the increasingly ubiquitous Nordic noir dramas taking over our TV screens – so you may be surprised to learn that it's the experience of one of the subjects in a recent University of Oxford study! Olivia Faull and colleagues from the Oxford Centre for Functional Magnetic Resonance Imaging of the Brain (based in the Nuffield Department of Clinical Neurosciences) devised an experiment to look at what is happening in the brain when we might be about to become breathless. And the results have striking ramifications that will help us better understand – and may eventually lead to new treatments for –asthma and other chronic respiratory disorders.
Asthma costs the NHS £1bn a year, and the economy a further £2bn, due to time off sick (Asthma UK). It has long been suspected that some cases of asthma may be made worse by stress and worry. Sometimes breathlessness is out of proportion with what is actually happening physiologically in the lungs. In some people anxiety or worry can even bring on an asthma attack. Researchers in Oxford became interested in what is happening where in the brain when this reaction occurs.
A normal functioning PAG is clearly a good thing. We need to know when we are in danger, whether from something we could run away from – such as a hungry lion – or something we can't escape but could endure, such as becoming breathless. But what happens when things go wrong?
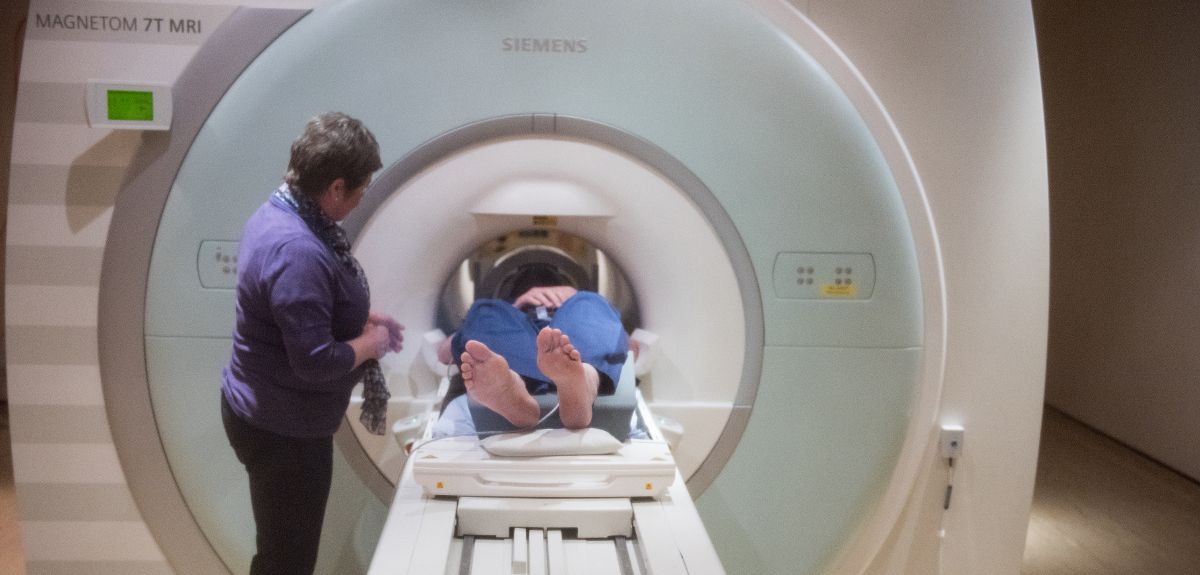
Scientists have known for some time that a tiny part of the brain called the periaqueductal gray (or PAG for short) plays an important role in how we perceive threat. Animal studies have revealed this bundle of cells in the brainstem to be the interface between automatic processes – such as breathing and heartbeat – and consciousness. The PAG is a group of cells ('grey matter') less than 5mm in diameter. Historically it has been very difficult to study in humans because it is so small and buried so deep. But the Oxford team managed to isolate the PAG using state-of-the-art magnetic resonance imaging (MRI) with super fine resolution.
Olivia and colleagues scanned a group of healthy volunteers in the ultra high-field 7 Tesla MRI scanner. The volunteers wore a breathing system similar to a snorkel, that could be altered to produce a resistance when subjects breathed in (like breathing through a very narrow straw). During the scan, subjects looked at a screen that showed three different symbols at various times. Eventually the subjects learnt the meaning of the symbols – for instance the triangle meant that nothing would happen and they could breathe normally, and the star meant that their air would definitely be restricted and they would become breathless.
Volunteers therefore learned when they may be about to find it difficult to breathe. Olivia was then able to look at what was happening in the PAG both when people thought they might become breathless, as well as during the difficult breathing itself. Olivia wanted to know what was happening when people anticipate breathlessness, to better understand the stress and anxiety that exacerbate it. The study found that averaged over all participants, a particular subdivision of the PAG (called the ventrolateral column) became active when people anticipated that they might become breathless, and another subdivision (called the lateral column) became active while they were actually breathless. This means that different subdivisions of cells within the PAG are doing different things throughout the course of breathlessness.
A normal functioning PAG is clearly a good thing. We need to know when we are in danger, whether from something we could run away from – such as a hungry lion – or something we can't escape but could endure, such as becoming breathless. But what happens when things go wrong? It could be that in people who are hyper-sensitive to threats, the function of the PAG or its communications to the rest of the brain are altered. For example, some people with asthma may get very stressed if they can't find their inhaler, and this may even bring on an attack: perhaps the PAG is telling them that they are in danger of becoming breathless (even if, physiologically, at that moment they are breathing normally).
Now that this ground-breaking MRI experiment has enabled researchers to know where and how to look at the PAG, they can carry out further studies to find out more about asthma and other conditions where the physiology doesn’t match the perception – such as chronic pain or panic disorders. Such work could lead to the development of new treatments, to see whether they have any effect on this tiny, hitherto inaccessible part of the brain. These could be new medicines or new behavioural interventions such as as mindfulness or cognitive behavioural therapy, or combinations of both.
The full article is published in the journal eLife.
Today poetry fans around the world are celebrating World Poetry Day.
To mark the day, we asked poetry experts from our English Faculty and Faculty of Medieval and Modern Languages about their own research into poetry, and what poems they recommend we should read today.
Later in the article, Professor Simon Palfrey of the English Faculty explains his collaborative scholarly and artistic project Demons Land: A Poem Come True.
Before that, Philip Bullock (Professor of Russian Literature and Music) and Alexandra Lloyd (Lecturer in German at St Edmund Hall and Magdalen College, University of Oxford) who lead the Oxford Song Network at The Oxford Research Centre in the Humanities (TORCH), give their take on World Poetry Day:
Arts Blog: What is the purpose and remit of the network?
PB: I think we say something on our website about the network – that it ‘explores the interaction of music and words in the nineteenth- and twentieth-century European song tradition’. But that’s incredibly complicated, as you might imagine. Trying to find a common language that brings together musicologists, linguists, historians and performers is one of the major challenges, and we’ve brought together a wide range of scholars from different fields in order to try to establish some common research questions and discuss how we each think about song (we’ve even pushed our period boundaries by talking to some classicists too).
We’ve also experimented with a number of different formats. We’ve had some more formal, conference-style events, often linked with the Oxford Lieder Festival, where people talk about their own research in depth. But we’ve also had smaller discussion groups in which we hear each other’s work in progress, and that’s a great opportunity to open things up for further discussion.
And this term, we’ve held a couple of workshops with current Oxford students and leading experts from outside the university – Helen Abbott from Sheffield, and Natasha Loges from the Royal College of Music – in order to explore the relationship, and sometimes even the tension, between poetry and music in song, to ask how we might translate song lyrics into English, and to explore what kind of knowledge and experience singers and pianists need to have in order to put across the meaning of a song to an audience that might not necessarily understand the language in which a song is sung.
A rather selfish reason for putting the network together was to get some feedback on a book I'm currently trying to write on Russian song, and I must say that I've always come away from every event buzzing with new ideas and angles to explore in my writing.
AB: What do you think of the way poetry is approached in schools and in the media? How would you change this?
PB: I think poetry can sometimes seem terribly formidable, and people think that studying it often involves learning lots about the complex meanings of words and all the hidden references and technical tricks that poets use to work their magic. That's all true, and it’s an important feature of how I teach poetry to my own students. But I sometimes think we forget the physical, embodied side of poetry – words that are spoken, or sung by a living, breathing human being.
We've rather lost the habit of memorising and reciting poetry (at least in the UK – Russians still do it with a passion), and with that, we’ve lost sight of poetry as a kind of performance, where sounds and sensations are as important in creating a relationship with the audience as the words on the page are. One of the exciting things about song is that it can bring poetry alive in the most intense way imaginable – we’re not just hearing a particular composer’s take on a poem, but a performer’s entire involvement with both the words and the music.
AL: I'd second what Philip writes about the embodied side of poetry. The expressiveness of sounds, and the feelings we encounter – emotional, but actually also physical – are part of the experience it’s easy to overlook sometimes. It's always a wonderful moment when students, for example, discover enjambment (the continuation of a sentence beyond the end of the line) – the breathlessness experienced by the reader roots the poetry in something beyond the intellectual.
Poems are not, and should not be taught as, collections of printed words on the page, any more than music is. For instance, listening to different composers’ settings of one poem can reveal so much about the original text by drawing attention to its different parts.
AB: What would you like people to take away from World Poetry Day?
PB: Thinking just about music for a moment, I’d like to suggest that song represents a wonderful form of imaginary travel. Listening to a Schubert setting of Goethe, a Glinka setting of Pushkin, or a Debussy setting of Baudelaire allows us to imagine not just very different historical periods, but totally new linguistic and cultural worlds.
As a linguist, I worry that not enough people study foreign languages, whether as part of the school and university curriculum, or simply for pleasure and enjoyment. But it’s not true that we live in a monolingual culture – we’re surrounded by other languages, some of them spoken by people who’ve moved here and brought their culture with them, and others that have been imported in the form of subtitled films, surtitled operas or bilingual programmes for song recitals.
My first encounter with German was falling in love with Schumann Lieder as a melancholy teenager, and I first began to learn Russian by deciphering the texts of the poems that Shostakovich set to music – they were very much the passport to my later life as a linguist and every bit as important as the fat novels I also love reading.
AL: I'd like to emphasise the idea that poetry is ubiquitous, particularly in music. When David Bowie died in January I watched the video of his final single ‘Lazarus’, released just a few days earlier. I was struck immediately by echoes of Heinrich Heine’s poem ‘Wie langsam kriechet sie dahin / Die Zeit, die schauderhafte Schnecke!’ (‘How slowly she creeps along, time, the loathsome snail’) from his cycle ‘Zum Lazarus'.
As with Bowie's character in the video, Heine spent the last eight years of his life bedridden, suffering from paralysis and confined to what he called his 'mattress grave'. These two verses about mortality - one from the mid-19th century, one from the early 21st - give us perhaps a sense of the connectedness of the human condition and the role of the arts and poetic expression in confronting that.
Would you like to suggest a poem for our readers to read today?
PB: I've recently discovered Japan, and although I can’t speak a word of the language, I’m really enjoying discovering its literature in translation. Basho’s frog haiku is terribly clever – and has been obsessively translated in an attempt to fathom its many secrets. It's also about sound, so ideal for someone like me, who’s interested in poetry’s musicality.
AL: I'm also part of the team that runs the Oxford German Network. Our national competition last year was on the theme of poetry and our website has a feature with lots of suggestions for reading.
For today, I'd suggest reading Lewis Carroll's poem 'Jabberwocky' - it's such a wonderful example of how 'nonsense' has meaning through sound and performance. There are also plenty of translations of it online - from the 'Jammerwoch' to 'Siaberwoci' to 'El Dragobán'...
 Demons Land
Demons LandSimon Palfrey, Professor of English Literature at Oxford University, leads a collaborative scholarly and artistic project inspired by Edmund Spenser's Faerie Queene, which Professor Palfrey describes as 'perhaps the single greatest poem of the English Renaissance'.
Arts Blog: Why is Fairie Queene significant?
SP: Edmund Spenser's Faerie Queene is perhaps the single greatest poem of the English Renaissance. I see it as a hallucinogenic masterpiece, erotic, ravishing, strange, and frequently very savage. Inspired by militant Protestant zeal, the poem was written in Ireland during the 1580s and 1590s, when Spenser served the English crown during the most violent years of the Elizabethan conquest. It presents an unbuilt world, and asks on what principles we might create a virtuous person and a reformed society.
Spenser's mission in Ireland failed. His poem both reflects and tries to redeem this failure, offering a model of the necessary future as much as a diagnosis of the present. Hence the imaginative premise of our project: that subsequent global history, a repeating mission of conquest, education, and colonization, can be understood as a tale of this poem coming differently, imperfectly to life. It has long been understood that the *Faerie Queene*, in its claim to change or to model lives, is an exemplary Christian humanist poem. In our project, FQ becomes the text of unfinished modernity.
Tell us about Demons Land?
Demons Land: A Poem Come True is a collaborative scholarly and artistic project telling the story of an island in which Spenser's poem comes beautifully and terribly to life. This is the project of the Collector, a Romantic who around 1800 vowed to remake an island at the bottom of the world into a poetic utopia. Demons Land becomes a shadow history of Britain's most notorious colony, the prison island called Van Diemens Land.
Like Spenser's mission in Ireland, the Collector's dream failed: not because his world failed to be like the poem; but because both the poem and the land were other than he thought. They had indigenous energies, lives, untapped implications that his discipline hadn't imagined.
The questions we ask are very basic. We are all familiar with the idea that a poem might reflect or record history. But what if it predicts history? What if history is itself structured like a poem? And we can extend these questions to life itself: what if lives happen as they do in poems, where they only have existence if they are seen, or only matter if they are sympathized with?
What if each individual life is not a self-sufficient experience, but an allegory of something other? What if metaphors are true, or life is organized in rhymes, stanzas, endlessly repeating rhythms? The question becomes: what does it mean (for society, or history, or a life) for a poem to come true?
Questions such as these cannot really be tested in conventional scholarly forms. They need a correspondent creative experiment. So the Demons Land project explores how different crafts and disciplines - poetry, painting, film, music, masks, puppetry, and creative literary criticism - can combine to embody a poetic vision. All of this will come together in an exhibition/installation telling the history of the experiment.
How do their imagined worlds differ?
Demons land is at once a repetition, an interpretation, a subversion, and a radical modernisation of Spenser's poem. *The Faerie Queene* is notoriously unfinished. Demons Land continues the story, and purports to complete the poem, by means of a simple premise: that FQ is the prophetic text of western modernity, coming imperfectly, differentially true throughout the dominions conquered or settled by the English.
Demons Land is the epitome of this history, being the suppressed pre-history of Van Diemens Land, which itself echoes the earlier histories of Ireland and America. History is thus structured recursively, like a poem: Demons Land repeats itself to this day.
Hence the fictional postulate of our project: that a contemporary woman discovers a store of texts and paintings deriving from Demons Land, and undertakes to recover and publicize this unknown history. But then she repeats the story in less predicted ways as well - like the Collector, she begins to be possessed by it, and to identify in personal and even perverse ways with the figures in FQ/Demons land.
What will the product of your research project be, and when/where can we see it?
The main products will be the exhibition, its films and paintings, and a book I am writing telling the history of Demons land. As well as an online version of the exhibition, we will exhibit in locations whose own history speaks to our project, adapting our narrative to each host. The first showing will be in the gardens and temples of Stowe National Trust, designed in the early eighteenth century as an architecturalised Faerie Queene - like Demons Land, a place made in the image of the poem, as an act of political critique and fantastic idealism.
The second showings will be in Scotland, in the Gothic Mount Stuart house on Bute - another monument of beleagured idealism, and an island whose semi-disappeared history mirrors that of Demons Land - and in Glasgow, the great port of empire.
What would you like people to take away from World Poetry Day?
That poetry speaks directly to the possibilities - beautiful and terrifying - of life and history; that good poetry is always unfinished, awaiting and adapting to new readers.
A trek to Everest base camp is helping Oxford University researchers investigate the links between heart failure and the low oxygen levels suffered by patients with a range of serious diseases.
Dr Cameron Holloway, Dr Nick Knight and Dr Andrew Murray from Oxford University's Department of Physiology, Anatomy and Genetics and the Oxford Centre for Clinical Magnetic Resonance Research were among several hundred volunteer hikers walking to the foot of Mount Everest to study the body’s response to the thin air.
The team wanted to simulate the condition of hypoxia – when the body or part of the body is deprived of sufficient oxygen. Patients with pneumonia, smoking-related diseases and some forms of heart failure suffer hypoxia.
It was Dr Holloway’s first experience of such a severe climate and he was startled by some of the findings. Among the most significant were changes to blood oxygen levels and energy synthesis.
‘I was amazed at how low the arterial oxygen levels fell in our blood,’ Dr Holloway said. ‘Saturation was in the 70 and 80 per cents during simple exercise at altitude when normally you would get worried if it dropped from normal at 98 per cent to 93 per cent.'
‘Usually that level isn’t compatible with life. If someone came in with levels that low we would rush them into intensive care.’
Another ‘huge shock’ was the 25 per cent drop in the cardiac phosocreatine/adenosine-triphosphate (PCr/ATP) ratio – a measure of the amount of energy available to the heart.
‘People with heart disease often have this ratio impaired. We experienced similar impairment, even reaching the levels of heart failure. We don’t know if it was due to adaptation to low oxygen or showed that our hearts were not coping.’
Dr Holloway’s study of 14 of the volunteers ran alongside a larger research project by Caudwell Xtreme Everest, part of the UCL Centre for Altitude, Space and Extreme environment medicine (CASE). The findings were published recently in The FASEB Journal.
Before leaving for Nepal, participants underwent wide-ranging tests, including assessments of heart, vascular, brain and exercise performance. Blood and other tests were carried out at several points during the 11-day ascent from Lukla’s Tenzing-Hilary Airport at 2,850m to 5,360m base camp.
The initial tests, which took place in Oxford, were repeated within 48 hours of the group’s return from Everest and carried out again six months after the trek ended. By then all changes to the heart and energy levels had returned to the pre-trek baseline.
Dr Holloway suspects that the findings witnessed during the Everest trip may have parallels with the cause of some forms of heart failure:
‘At base camp the symptoms we had, including breathlessness and exercise intolerance, were similar to those experienced by heart failure patients.'
‘Even a small amount of exercise was really difficult. That’s what people have to deal with when they have pneumonia or other diseases.’
Dr Holloway hopes the lessons from the study will improve care for critically ill adults and children, and even babies in incubators.
‘Now we are looking at heart failure patients to see if low oxygen is the problem and if changing oxygen pathways could improve the lives of heart failure patients. We also need to work out what is behind individual differences in the changes people experience as a result of low oxygen.’



 What Louise Thompson’s campaign tells us about the national maternity crisis
What Louise Thompson’s campaign tells us about the national maternity crisis Celebrating 25 Years of Clarendon
Celebrating 25 Years of Clarendon  Learning for peace: global governance education at Oxford
Learning for peace: global governance education at Oxford  What US intervention could mean for displaced Venezuelans
What US intervention could mean for displaced Venezuelans  10 years on: The Oxford learning centre making an impact
10 years on: The Oxford learning centre making an impact Oxford and The Brilliant Club: inspiring the next generation of scholars
Oxford and The Brilliant Club: inspiring the next generation of scholars New course launched for the next generation of creative translators
New course launched for the next generation of creative translators The art of translation – raising the profile of languages in schools
The art of translation – raising the profile of languages in schools