
Image credit: Shutterstock
Maths gives new insights into damage caused during brain surgery
It might sound alarmingly similar to the prehistoric procedure of trepanning, but decompressive craniectomy – the removal of a large part of the skull to reduce swelling in the brain – is still used as a last-resort treatment for traumatic brain injury or stroke by surgeons around the world.
Perhaps unsurprisingly, the complication rate of this major operation is high. As the brain 'mushrooms' out of the skull following the removal of bone from the skull, stresses and stretches placed on other parts of the brain can lead to neuronal damage and potential long-term disability.
But this is no longer just a challenge for neurosurgeons. Mathematicians are now able to study and model the impact of surgery at organ level, developing a more specific picture across the whole brain. Professor Alain Goriely of Oxford Mathematics and Stanford colleagues Professor Ellen Kuhl and Dr Johannes Weickenmeier have looked at the issue by studying a standard physical problem: the problem of bulging in soft solids.
Bulging takes place when a material swells while constrained – except at an opening, as seen when the skull is opened during decompressive craniectomy and the brain bulges out of the newly created hole. This can create deformations in another part of the brain, away from the immediate incision.
 Researchers used high-resolution magnetic resonance imaging to create craniectomy models.
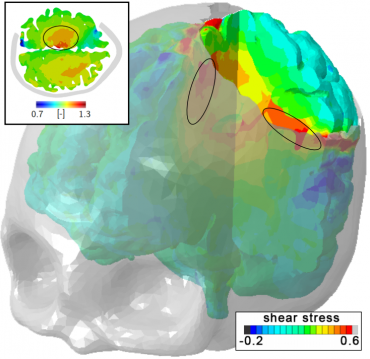
Researchers used high-resolution magnetic resonance imaging to create craniectomy models.Image credit: Alain Goriely
To quantify possible deformations inside the brain, the team created a personalised craniectomy model from high-resolution medical resonance imaging. Their study reveals three mechanisms of failure that could denote damage beyond the initial incision point: axonal stretch in the centre of the bulge (axons are nerve fibres that carry impulses away from nerve cells), axonal compression at the edge of the craniectomy, and axonal shear around the opening. Strikingly, even small amounts of swelling can induce axonal strain in excess of 30% above reported damage thresholds in patients.
Professor Goriely said: 'This research points towards a possible way of proving and identifying long-term damage to the brain following decompressive craniectomy. Indeed, this theoretical study is a first step towards gaining better insight into the complex mechanisms underlying craniectomy and opens the door for systematic personalised studies of craniectomy in patients. The next step is to combine this theoretical work with experimental and clinical work to enable surgeons to provide better-informed and more successful treatments.'