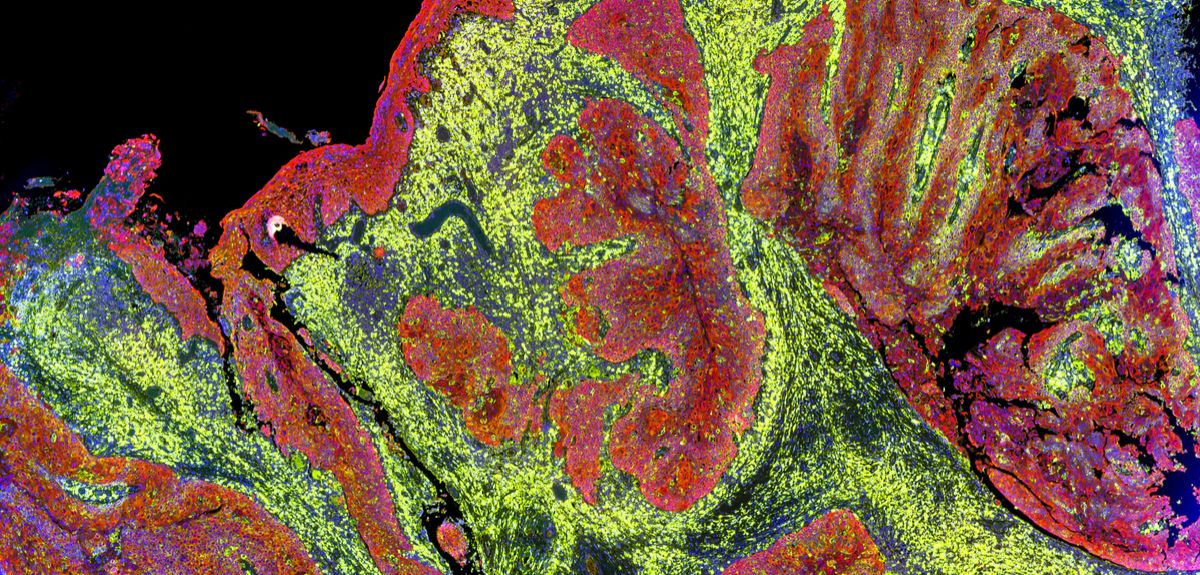
Image credit: Shutterstock
Breast cancer study suggests review of treatment length
A new study published in the New England Journal of Medicine, funded by Cancer Research UK, has found that the risk of breast cancer recurring persists undiminished for at least 20 years after diagnosis, suggesting that hormonal treatments should continue for even longer to reduce the risk of late recurrence.
The Early Breast Cancer Trialists’ Collaborative Group, an international team of investigators based at the University of Oxford, pooled data from over 60,000 women in 88 clinical trials who had been diagnosed with estrogen receptor positive breast cancer between 1976 and 2011, and prescribed anti-estrogen therapy, such as tamoxifen or an aromatase inhibitor, for 5 years. These women who had no recurrence in the first 5 years, then stopped treatment and their progress was followed for up to 15 further years.
Over 11,000 had a recurrence of cancer at a distant site, such as the bone, liver, or lung, with the risk of recurrence during each subsequent year (from years 5-20) remaining about constant. The risk of recurrence was strongly related to the presence and number of involved axillary lymph nodes at diagnosis, as well as the size and pathologic grade of the cancer. The highest risk of recurrence was among women with 4 or more involved axillary nodes, who had a 40% risk of a distant cancer recurrence by year 20 after first diagnosis. Women at the lowest risk, ie those with small, low grade cancers and no spread to the nodes, had a much lower 10% risk of distant spread by year 20.
Professor Daniel F Hayes, senior author of the study from the University of Michigan Comprehensive Cancer Center, commented: 'We now know that continuing to take anti-estrogen therapy beyond five years can reduce the risk of recurrence but it’s hard to know whether these benefits will outweigh the possible side effects of continuing treatment. This study shows us what the risk would be if women stop treatment at 5 years and this gives us a good idea of what the likely benefits of continuing therapy would be for each individual patient and so helps them and their health care providers decide whether to continue treatment.'
Dr Hongchao Pan, lead author from the University of Oxford also commented: 'It is remarkable that breast cancer can remain dormant for so long and then spread many years later with this risk remaining the same year after year and still strongly related to the size of the original cancer and whether it had spread to any lymph nodes. This improved understanding of the factors that raise the risk of a late recurrence will help women and their doctors make individual decisions on how long to continue hormonal treatment.'
Professor Richard Gray, another lead author from the University of Oxford also commented: 'To assess 20-year risks, we studied women who received their breast cancer diagnosis many years ago, and we know that treatments have improved since then so women who were diagnosed more recently may be reassured that recurrence rates will be somewhat lower for them. This study does show, though, why women with estrogen receptor positive breast cancer should at least consider taking anti-estrogen therapy beyond five years and may also help motivate women who are experiencing side-effects to persist with treatment.'
Professor Arnie Purushotham, Cancer Research UK’s senior clinical adviser, said: 'This research shows that stopping hormone treatment at 5 years leaves women with an ongoing risk of breast cancer coming back in the distant future. It’s important to point out that since this research began, new drugs are being used to treat breast cancer that are better at preventing recurrence than those given to most women in this study. It’s vital that work continues to better predict which cancers might return. We also need to know what the difference for women might be in taking hormone therapies for 10 years instead of 5, the side-effects and how this affects patients' quality of life.'
 Statins do not cause the majority of side effects listed in package leaflets
Statins do not cause the majority of side effects listed in package leaflets
 Activism proves a stimulating topic at Sheldonian Series event
Activism proves a stimulating topic at Sheldonian Series event
 New Oxford-led initiative launches to train future leaders in transformative technologies for pharmaceutical research
New Oxford-led initiative launches to train future leaders in transformative technologies for pharmaceutical research