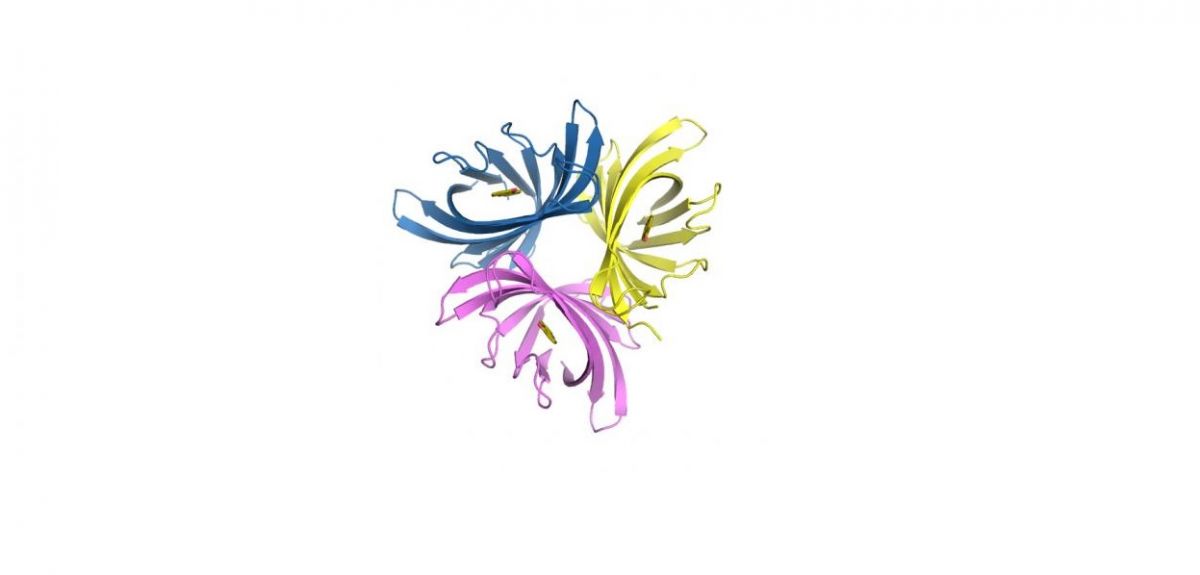
Image credit: Kyle Costa/Caltech
Protein disrupts infectious biofilms
This post originally appeared on the Caltech website. Author: Lori Dajose.
Many infectious pathogens are difficult to treat because they develop into biofilms, layers of metabolically active but slowly growing bacteria embedded in a protective layer of slime, which are inherently more resistant to antibiotics. Now, a group of researchers at Caltech and the University of Oxford have made progress in the fight against biofilms. Led by Dianne Newman, the Gordon M. Binder/Amgen Professor of Biology and Geobiology, the group identified a protein that degrades and inhibits biofilms of Pseudomonas aeruginosa, the primary pathogen in cystic fibrosis (CF) infections.
The work is described in a paper in the journal Science.
'Pseudomonas aeruginosa causes chronic infections that are difficult to treat, such as those that inhabit burn wounds, diabetic ulcers, and the lungs of individuals living with cystic fibrosis,' Newman says. 'In part, the reason these infections are hard to treat is because P. aeruginosa enters a biofilm mode of growth in these contexts; biofilms tolerate conventional antibiotics much better than other modes of bacterial growth. Our research suggests a new approach to inhibiting P. aeruginosa biofilms.'
The group targeted pyocyanin, a small molecule produced by P. aeruginosa that produces a blue pigment. Pyocyanin has been used in the clinical identification of this strain for over a century, but several years ago the Newman group demonstrated that the molecule also supports biofilm growth, raising the possibility that its degradation might offer a new route to inhibit biofilm development.
To identify a factor that would selectively degrade pyocyanin, Kyle Costa, a postdoctoral scholar in biology and biological engineering, turned to a milligram of soil collected in the courtyard of the Beckman Institute on the Caltech campus. From the soil, he isolated another bacterium, Mycobacterium fortuitum, that produces a previously uncharacterised small protein called pyocyanin demethylase (PodA).
Adding PodA to growing cultures of P. aeruginosa, the team discovered, inhibits biofilm development.
'While there is precedent for the use of enzymes to treat bacterial infections, the novelty of this study lies in our observation that selectively degrading a small pigment that supports the biofilm lifestyle can inhibit biofilm expansion,' says Costa, the first author on the study. The work, Costa says, is relevant to anyone interested in manipulating microbial biofilms, which are common in natural, clinical, and industrial settings. 'There are many more pigment-producing bacteria out there in a wide variety of contexts, and our results pave the way for future studies to explore whether the targeted manipulation of analogous molecules made by different bacteria will have similar effects on other microbial populations.'
While it will take several years of experimentation to determine whether the laboratory findings can be translated to a clinical context, the work has promise for the utilisation of proteins like PodA to treat antibiotic-resistant biofilm infections, the researchers say.
'What is interesting about this result from an ecological perspective is that a potential new therapeutic approach comes from leveraging reactions catalysed by soil bacteria,' says Newman. 'These organisms likely co-evolved with the pathogen, and we may simply be harnessing strategies other microbes use to keep it in check in nature. The chemical dynamics between microorganisms are fascinating, and we have so much more to learn before we can best exploit them.'
The paper is titled 'Pyocyanin degradation by a tautomerizing demethylase inhibits Pseudomonas aeruginosa biofilms.' In addition to Costa and Newman, other co-authors include Caltech graduate student Nathaniel Glasser and Professor Stuart Conway of the University of Oxford. The work was funded by the National Institutes of Health's National Institute of Allergy and Infectious Diseases, the National Science Foundation, the Howard Hughes Medical Institute, the Molecular Observatory at the Beckman Institute at Caltech, the Gordon and Betty Moore Foundation, and the Sanofi-Aventis Bioengineering Research Program at Caltech.