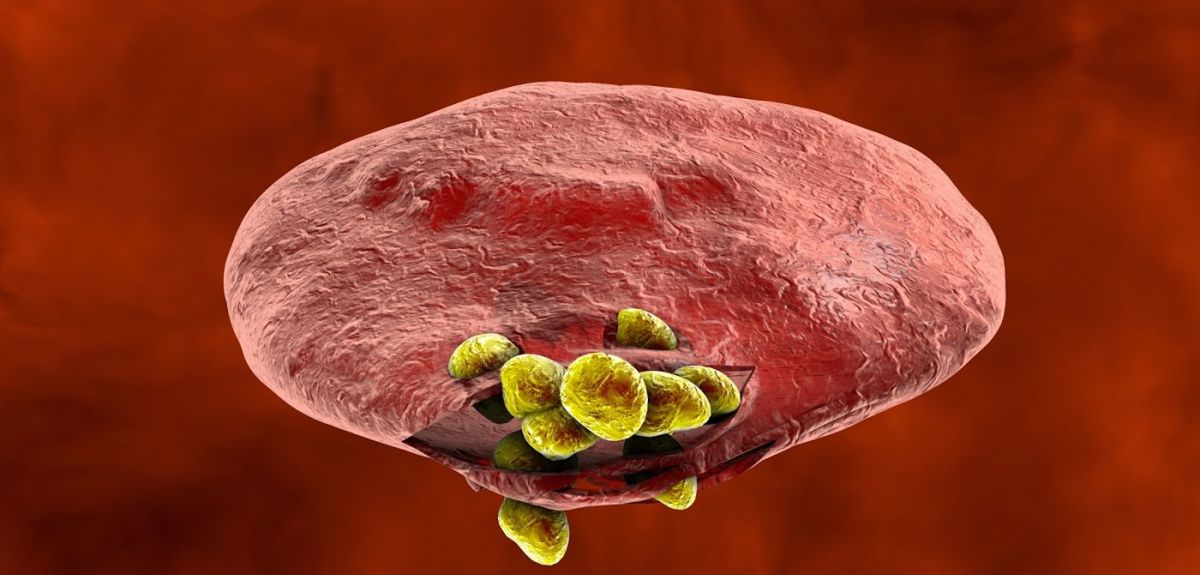
Source: Kateryna Kon/ Shutterstock
MalariaGEN - beating Malaria through genetics
Despite huge efforts to treat and eradicate the disease, in 2013, 198 million people were infected with Malaria. 584,000 died. More than 525,000 of those deaths were African children aged under five.
Researchers are looking for new ways to target malaria, including vaccines and drugs, and important clues may lie in genes – our genes, the parasite’s genes and even those of the mosquito that transmits the parasites from person to person. A team based in Oxford and at the Wellcome Trust Sanger Institute, just outside Cambridge, are working together with scientists and clinicians in more than 40 malaria-endemic countries to integrate epidemiology with genome science.
This is the Malaria Genomic Epidemiology Network (MalariaGEN), a global researcher community aiming to understand the genetic diversity in the human host, the malaria parasite and the mosquito vector. Last year the science blog spoke to the team about some of their initial findings, but their research has continued.
In the first of two interviews about research from MalariaGEN, we look at a study published in Nature, which found that genetic variation at a particular place in the human genome is responsible for protecting some children from developing severe malaria. The Oxford Science Blog put some questions to Dr Chris Spencer and Dr Kirk Rockett, two of the team behind the study. Their research reinforces earlier findings about a long-standing evolutionary battle between the human and malaria parasite genomes, each trying to outfox the other (the so-called Red Queen Hypothesis first coined by Leigh Van Valen in 1973).
OxSciBlog: In effect, some people are more resistant to malaria than others?
Answer: Yes. In regions where malaria is endemic, people are exposed to malaria (get bitten by mosquitoes carrying malaria) all the time. Most people will develop some form of illness with the classical symptoms (fever, sweating and chills) and sometimes this will develop into a severe, life-threatening disease. Young children are most at risk from severe illness as they have not yet had time for their immune systems to protect them, such that by adulthood they are less likely to become ill yet may be infected.
However, it is clear that some children are less likely to develop illness or severe disease than others. Some of these children have underlying conditions such as G6PD deficiency, thalassemia or sickle cell trait. All of these have been shown to have defined genetic polymorphism (mutations/changes). Studies such as ours allow estimates to be made of how protective these genetic changes are; individuals with sickle-cell trait for example are about 10 times less likely to develop any degree of illness from a malaria infection wherever they live compared with the general population.
This is a particularly strong effect and the other known protective genetic changes are providing generally between 20% and 50% protection. The other well-known example is the ABO blood group, where the genetic polymorphism which determines the O blood group also provides protection against malaria.
Questions remain as to whether there are other common genetic changes that protect from malaria and what happens in people with more than one polymorphism.
OSB: You carried out a genetic association study – what is that?
We've performed this test at over 10 million polymorphisms across the whole genome in thousands of individuals across Africa.
A: Don’t tell anyone, but a genetic association study is a very simple experiment! For the polymorphism you are interested in you measure which alleles of the polymorphism individuals carry.
For example, the sickle cell polymorphism has 2 alleles, either an A or a T, and we measure whether people have 2 copies of the A, 2 copies of the T or one copy of each. We then simply look to see if any of these alleles occur less often in children that develop severe disease than they do in the general population. If an allele is at a lower frequency in children with severe disease the implication is that this allele is protective.
The experimental and statistical complications come from the fact that we’ve performed this test at over 10 million polymorphisms across the whole genome in thousands of individuals across Africa and this generates a huge amount of data.
OSB: What did you find?
A: Our study identifies several new DNA variants that have a substantial protective effect for developing severe malaria. For one polymorphism in East Africa, the protective allele almost halved a child’s chances of developing life-threatening malaria. This DNA variant occurs near a set of genes belonging to the glycophorin family of genes, which express proteins on the surface of the red blood cells.
The discovery potentially links malaria susceptibility to one of only six clear examples of combinations of alleles (haplotypes) that have been maintained in human populations by natural selection. These alleles are thought to predate the time at which we split from chimpanzees some 5 million years ago. The genome is a big place and to find a haplotype of this kind slap-bang next to novel malaria susceptibility alleles is surprising, not least because ABO blood groups also show common polymorphism with chimpanzees. It is possible that susceptibility to malaria is part of the evolutionary mechanism sustaining alleles in the human population that would otherwise be lost by chance.
OSB: What are the implications for modern malaria research?
These genetics changes, whatever they do, have a major impact on the progression of infection either down the path to recovery, or to life-threatening disease.
A: Identifying the specific DNA variants that influence risk is the first step on a scientific path to understanding the mechanisms of disease. We can’t yet be sure what molecular biology underlies the variants that we observed, but there is good evidence that it relates to the nearby glycophorin genes which, when expressed as proteins on the red blood cell surface, are known receptors for the malaria parasite that help them bind and enter the red cell.
This reinforces the need to understand these host-parasite interactions, and our study means that we can pinpoint particular genetic changes which are unequivocally important in the outcome of infections – this allows scientists to focus future research with much more confidence and precision. On the flip side this research will also help to understand more about and parasite and how it has evolved and is evolving.
Our observation in this large population study proves that in real-world settings (as opposed to in a laboratory) these DNA changes provide strong protection against severe malaria. Rather than guessing as to what the relevant molecular biology is in malaria infections, our study says that these genetics changes, whatever they do, have a major impact on the progression of infection either down the path to recovery, or to life-threatening disease.
 Genetic insights into our evolutionary battle with malaria
Genetic insights into our evolutionary battle with malaria