Research shows possible way to prevent degenerative eye condition
An Oxford University study has found that reducing the tendency of vitamin A to form toxic clumps could slow down a condition that leads to blindness in children and young adults.
People usually associate vitamin A as being good for the eyes, but the study found that in patients with Stargardt disease, vitamin A transforms into toxic compounds, which cause chronic inflammation, premature ageing of the retina and vision loss.
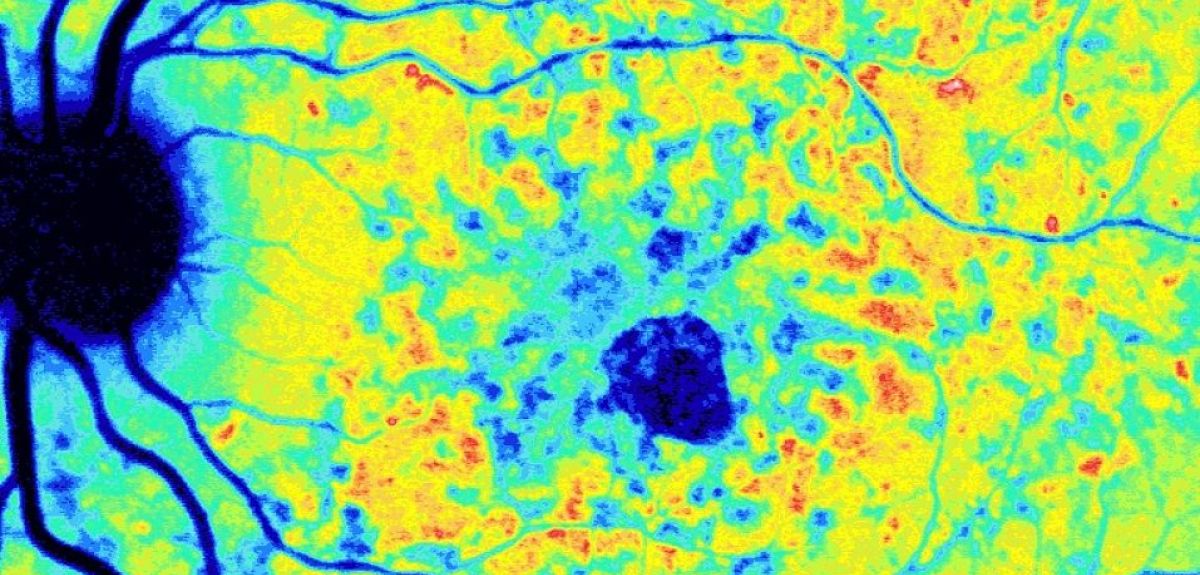
Stargardt disease affects around 1 in 10,000 people and begins in childhood, leading to progressive loss of central vision. The condition is linked to defects on a gene known as ABCA4. In Stargardt disease, the light-sensitive tissue in the back of the eye - the retina - ages prematurely and granules called ‘lipofuscin’ accumulate.
To date, there is no treatment for Stargardt disease, but a team led by Oxford University DPhil student Peter Charbel Issa (now a Professor at the University of Bonn), used genetically engineered mice to look at one possible cause of the premature aging of the retina in Stargardt disease. Collaborating with Dr Ilyas Washington, a chemist at Columbia University in New York City, the team hypothesised that the degeneration was triggered by the formation of toxic clumps derived from vitamin A, which form through a process called ‘dimerization’.
To test this theory they used a modified vitamin A, which had deuterium atoms in place of hydrogen at a critical position on the vitamin A molecule. The modified vitamin A was administered in the diet of mice with the Stargardt genetic defect. The incorporation of deuterium atoms on the vitamin prevented it from clumping. As a result, lipofuscin formation was dramatically reduced along with inflammation, and progression of Stargardt disease was prevented. The treatment was also shown to be safe in both mutant and normal mice.
Dr Charbel Issa said: ‘An important discovery was that Vitamin A dimerization is responsible for around half of the lipofuscin found in the RPE. While others had suggested it might be a cause, we have confirmed that it is an important factor. If we can reduce the rate at which vitamin A dimerizes, we could reduce the genetically-induced build-up of lipofuscin and slow down the progress of retinal degeneration.
‘We also wanted to check if the altered vitamin A could cause any side-effects in humans that might affect sight in another way, for example by damaging peripheral or low-light vision. However, tests showed that this was not the case – there was no adverse outcome in both normal and mutant mice fed the deuterated vitamin A’.
Prof Robert MacLaren, an eye specialist who supervised the project at the Nuffield Laboratory of Ophthalmology added: ‘Stargardt disease affects many children I see in my clinic and ABCA4-related retinal degenerations are also common in adults. The finding that a safe and simple dietary modification may help them is extremely promising. Dr Charbel Issa is to be congratulated for undertaking this incredibly detailed analysis that has provided further scientific validation of inhibiting vitamin A dimerization in this disease. We look forward to the next step of clinical trials.’
 Oxford tops European university rankings
Oxford tops European university rankings
 Researchers find reducing salt in everyday foods could prevent tens of thousands of heart attacks and strokes
Researchers find reducing salt in everyday foods could prevent tens of thousands of heart attacks and strokes